Aktis Oncology Pt 2: Alpha vs Beta Emitting Radionuclides $akts
Daughter nuclides, supply issues, nectin-4 beyond bladder cancers
I wrote two weeks ago on Aktis Oncology, focusing primarily on its miniprotein radioconjugate platform and why that’s a unique delivery approach. Delivery, however, is only one piece of the puzzle. Engineering the perfect method to get into cancerous cells won’t help much if you can’t deliver the correct toxic payload with it.
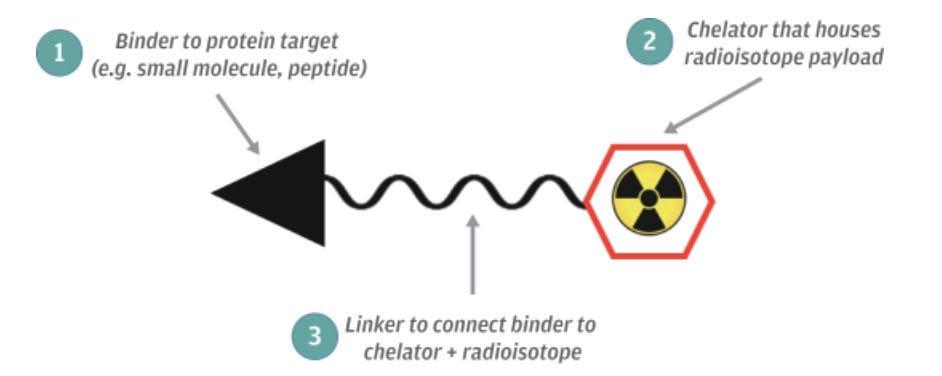
The general structure of a therapeutic radiopharmaceutical is well illustrated in RayzeBio’s S1 filing:1
The linker and chelator are critical pieces of radiopharmaceuticals, but aren’t a differentiated part of what Aktis is doing. Linkers keep the radionuclide (and, for typical ADCs, whatever the cytotoxic drug is) attached to the targeting agent until it is close to or inside the malignant cells. In the context of radiopharmaceuticals, chelators are used to prevent the radionuclide from spilling out of the therapeutic construct and affecting healthy tissue.
Where Aktis does start to differ from other companies is in its choice of radionuclide. The company is working on radiopharmaceuticals that use Actinium-225, an alpha-emitting isotope. This isn’t necessarily a unique approach (there are a number of companies trying this in clinical trials), but it’s not the one taken by FDA-approved Lutathera or Pluvicto.2 Both of these use Lutetium-177, a beta-emitting isotope. There are a few differences between alpha and beta particles:
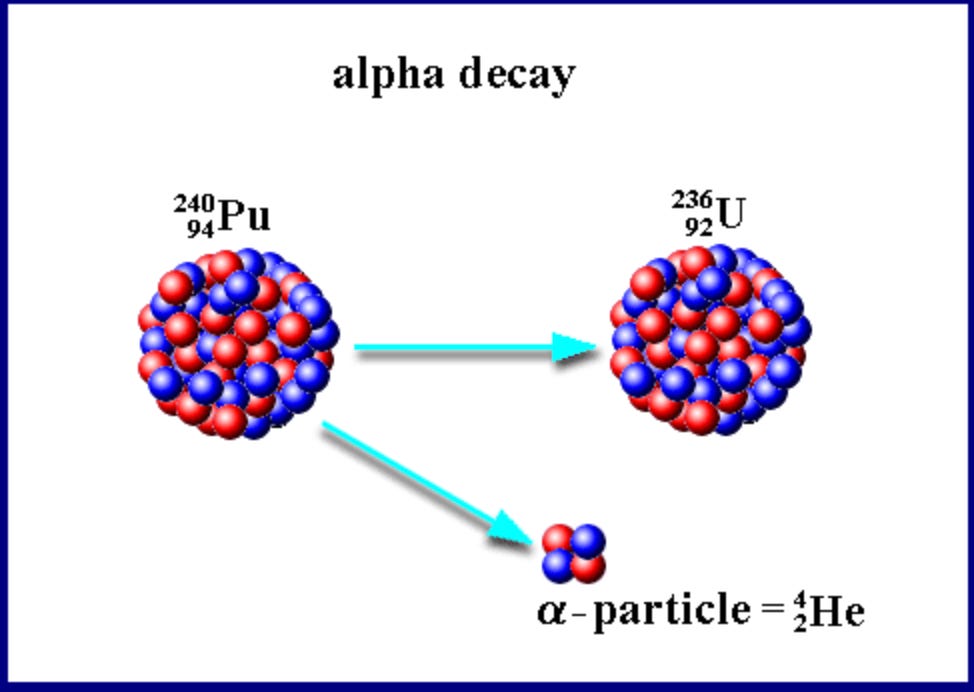
Beta-particles are made up of an electron; alpha-particles are two protons and two neutrons (and so look quite like a Helium ion). Consequently, alpha particles are much heavier.
Alpha particles cause double-stranded DNA breaks, beta particles cause single-stranded breaks. This could be why Lutathera and Pluvicto slow cancer progression but do not cure it. Single-stranded breaks are easier for cells to fix than double-stranded ones.
In layman’s terms, alpha particles have a more limited ‘blast radius’ compared to beta particles. The damage they cause is more severe but less widespread.
I won’t get into it here, but alpha particles remain effective in hypoxic tumor environments, an area where beta-emitters/traditional radiation treatments struggle. This isn’t really relevant to the purpose of this piece.
Historically, it was thought that alpha particles’ more limited radius meant they would be a fit for treating very small groups of cancerous cells but wouldn’t exert much impact on larger tumor sites. It’s turned out that these particles actually can significantly damage large tumors (see here and here), but it’s not entirely clear why.
Excitement about these alpha-emitting isotopes, and particularly Ac-225, took off after a 2016 paper detailed their effectiveness in treating two patients with metastatic castration resistant prostate cancer. These two patients either didn’t respond to beta-emitters or weren’t a good fit for them, and both responded remarkably well to treatment with peptide-conjugated Ac-225. These peptide targets aimed at PSMA, much like Pluvicto, and caused marked drops in PSMA positive lesions.
Regrettably, Ac-225’s promise was limited by severely constrained supply and concern about its radioactive decay chains. Ac-225 doesn’t really show up in nature so has to be created synthetically, which is quite a complicated process! Until recently it could really only be made in any notable-ish quantities at one location. The issue with Ac-225’s radioactive decay chain requires some explaining of radionuclides in general:
An element is defined by its atomic number, or the number of protons in its nucleus. This is the number right above an element’s name in the periodic table (Carbon has 6 protons, Calcium has 20, Lutetium has 71, Actinium has 89). Isotopes of an element all have the same number of protons, but a varying number of neutrons. When this ratio of neutrons to protons is unfavorable (the threshold here depends on the mass of the element), the isotope becomes unstable. Unstable isotopes don’t enjoy existing in that state, and so try to head towards stability. The process of radionuclides searching for stability is termed radioactive decay, and it is here that radioisotopes become useful for therapeutic purposes. During radioactive decay there’s an emission of energy (in our case an alpha or a beta particle), and, as a result of that emission of energy, the radionuclide becomes (most of the time) a different radionuclide/stable nuclide.3 It’s this emission of energy that can disrupt cancerous cells.
The nuclide that a radioisotope decays to is termed a daughter nuclide, and unfortunately these can cause problems. In the case of alpha-emitting particles, daughter nuclides ‘eject’ with so much energy that they can break out of the chelator and cause damage to healthy tissue.4 For Ac-225 specifically one of its daughter nuclides is Bi-213, which causes toxicity in the kidneys.
This daughter nuclide problem increases the importance of Aktis’ delivery platform. Antibodies come with two relevant downsides when it comes to alpha-emitting radioisotopes: they have a much longer half-life than peptides (think days to weeks rather than hours) and exhibit poor tumor penetration. The longer half-life is an issue because it means the antibody-conjugate is circulating through the healthy parts of a patient for an extended period of time. In other words, a patient is exposed to toxicity with no clinical benefit. For alpha-emitting particles this extended half-life becomes a double issue, as it gives daughter nuclides, particularly Bi-213, plenty of time to cause trouble for the kidneys. In the case of beta-emitting isotopes, antibodies’ poor tumor penetration theoretically matters less; with alpha-emitting particles, however, it means that they’re really not able to reach much of the tumor.
Miniproteins solve these issues. Their half-life is similar to that of peptides, and their size means they’re able to reach a lot of the tumor. Of course, the miniprotein doesn’t get rid of the fact that Ac-225 has problematic daughter nuclides. With the miniprotein approach, however, the radionuclide payload is rapidly delivered to cancerous cells. Consequently, radioactive decay predominantly occurs within these cancerous cells rather than out in the bloodstream, and one shouldn’t have to worry about systemic toxicity.
It’s worth noting here the uniqueness of Aktis’ approach. I mentioned above the case of two patients with metastatic prostate cancer. In that instance, a peptidomimetic (small molecule designed to mimic a peptide) was used to target the PSMA protein, and so half-life/daughter nuclides are less relevant considerations. Peptides/peptide-mimics have short half-lives, effectively get into the tumor, and get in fast enough that one doesn’t have to worry as much about daughter nuclides. The real constraint, then, for alpha-targeting therapies using a linear peptide/small-molecule conjugate has been around securing enough Ac-225 supply. Again, this is far from an easy problem to solve!5 It is, however, one problem less than what Aktis is trying to figure out. The company not only has to solve the supply bottleneck, but also has to design targeting molecules that aren’t antibodies but bind like antibodies. Without this, alpha-emitters remain out of reach for targeting proteins that are highly expressed on cancerous cells, but have a flattish surface rather than a clearly defined binding site.6
The final point worth making on Aktis is the amount the company is spending: typically companies don’t say they’ll burn 140-150mm advancing an ongoing Phase 1b trial! Typically companies also don’t run a Phase 1b trial with a target enrollment of 150 participants. For reference, RayzeBio, another alpha-emitting radiopharmaceutical player, enrolled 17 patients in a Phase 1b trial for its lead candidate and probably spent a tenth of what Aktis is planning to.
This isn’t an apples-to-apples comparison for a few reasons, but most notably because Aktis believes its lead candidate has broad applicability, and so is running its Phase 1b trial across multiple tumor types:
“Our lead product candidate, [225Ac]Ac-AKY-1189, was generated using our miniprotein radioconjugate platform and is designed to deliver 225Ac, a highly potent alpha-emitting radioisotope, to Nectin-4 expressing tumors. Nectin-4 is a cell surface protein found on a wide variety of tumors and has very limited expression in normal adult tissues. Nectin-4 is also the target of enfortumab vedotin, or Padcev, an approved ADC for the treatment of locally advanced and metastatic UC……..We believe AKY-1189, when conjugated to a radioisotope, has the potential to treat UC as well as other Nectin-4 expressing tumors”7
The choice to target patients with urothelial cancer makes sense. Padcev, which is mentioned frequently in Aktis’ S1 filing, was the first antibody-drug conjugate approved for the treatment of urothelial cancer. Padcev similarly targets the Nectin-4 protein, and has estimated peak annual sales of 7 billion USD (depending on who you ask!) There’s reason to be a tad skeptical, however, of AKY-1189’s applicability in other Nectin-4 expressing tumor types. The other Nectin-4 expressing cancer that Aktis mentions by name is triple-negative breast cancer (TNBC). While cancerous cells in TNBC often do express the Nectin-4 protein (this paper estimates Nectin-4 is expressed in 62% of TNBC cases), Padcev’s Phase 2 results for TNBC were on the disappointing end. Moreover, there are already approved ADCs for TNBC, most notably Trodelvy. Importantly, Trodelvy targets the Trop-2 protein, which is expressed in over 90% of TNBC cases. Quite a bit better than 62%.
The one very brief note I’d make on valuation is that it doesn’t necessarily make sense to evaluate these radiopharmaceutical companies based on their current clinical pipelines. Their supply chain/manufacturing capabilities very much come into play, which is something Eli Lilly and Bristol Myers Squibb both made clear in their Point Biopharma/RayzeBio acquisitions. This funnily enough means that one risk to valuation is that the alpha emitting isotope supply problem is solved a little too well, such that big pharma sees much less value in expertise/capabilities there.
Disclaimer: The information in this post is not intended to be and does not constitute investment or financial advice. You should not make any decision based on the information presented without conducting independent due diligence.
RayzeBio was acquired by Bristol Myers Squibb for 4.1 billion in late 2023.
Xofigo is an FDA approved therapeutic that does use Ac-225, but without an antibody or peptide conjugate. Xofigo was approved back in 2013, and hasn’t generated close to the same excitement as Lutathera/Pluvicto.
This radioactive decay chain will continue until the isotope eventually becomes stable.
This isn’t a problem for beta-emitting particles, as the daughter nuclides don’t eject with enough force to break out of the chelator.
RayzeBio had to pause enrollment in a phase 3 study because of Ac-225 supply constraints.
To be clear, Aktis isn’t the only company trying to figure out this problem. Bicycle Therapeutics is developing bicyclic peptides to leverage protein-protein intermolecular contacts. RayzeBio is using a macrocyclic peptide for its hepatocellular carcinoma candidate that targets GPC3.
Aktis S1, pg 6.


Really sharp analysis on the daughter nuclide constraint. The miniprotein angle is clever because it solves the Bi-213 kidney toxicity through rapid tumor delivery rather than just trying to engineer better chelators. I've seen simialr issues with longer half-life conjugates in radioimmunotherapy trials, where systemic exposure becomes the limiting factor. The skepticism around TNBC applicability feels spot on given that 62% vs 90% target expresion gap.