UniQure: (Hopefully) Progress on miRNA Therapeutics $qure
siRNA vs miRNA, the FDA, Exon 1 vs Allele-Specific
RNA-based therapies have been on a bit of an up and down trajectory over the past few years. On the one hand, Novartis recently announced its many billion-dollar acquisition of Avidity, which is developing RNA-based treatments for neuromuscular diseases. On the other, Moderna’s share price is down over 90% from its peak, the company scrapped its vaccine candidate for CMV in October, and HHS cancelled almost 500mm in mRNA vaccine contracts back in August. The general trend has been that excitement about mRNA-based infectious disease vaccines has waned considerably, but excitement about RNA-based therapeutics that modulate problematic mRNA expression is still there (said differently, if you’d gone long Alnylam and short Moderna five years ago you would’ve done very well).
An area where RNA hasn’t met much success yet is powering one-time treatments for genetic diseases. At first glance this makes sense: any therapeutic delivered in the form of RNA is inevitably going to be degraded by the body’s cellular machinery. RNA is inherently transient; it’s not supposed to exist forever. There’s a lot of work that goes into prolonging RNA therapeutics’ persistence in the human body, but the goal is to lengthen its existence, not make it last indefinitely.
Put differently, the goal of current RNA-based therapies is different from the goal of one-time gene therapies like Zolgensma or Elevidys. In those cases, the goal is to deliver a functional gene to the body, which will remain there permanently, and continuously be transcribed and then translated into a functional protein. In principle, however, gene therapies can be used to deliver more than only genes that will be translated into proteins. Plenty of genes are transcribed into something other than mRNA, and these other types of RNA can be incredibly useful! In theory, it’s possible to deliver a gene to a patient that would permanently produce a type of non-coding RNA. These therapeutics are probably best thought of as both gene therapies and RNA-interference therapies. While they would be delivered as genes, their end state means they’re taking advantage of the same mechanisms as companies like Alnylam or Arrowhead.
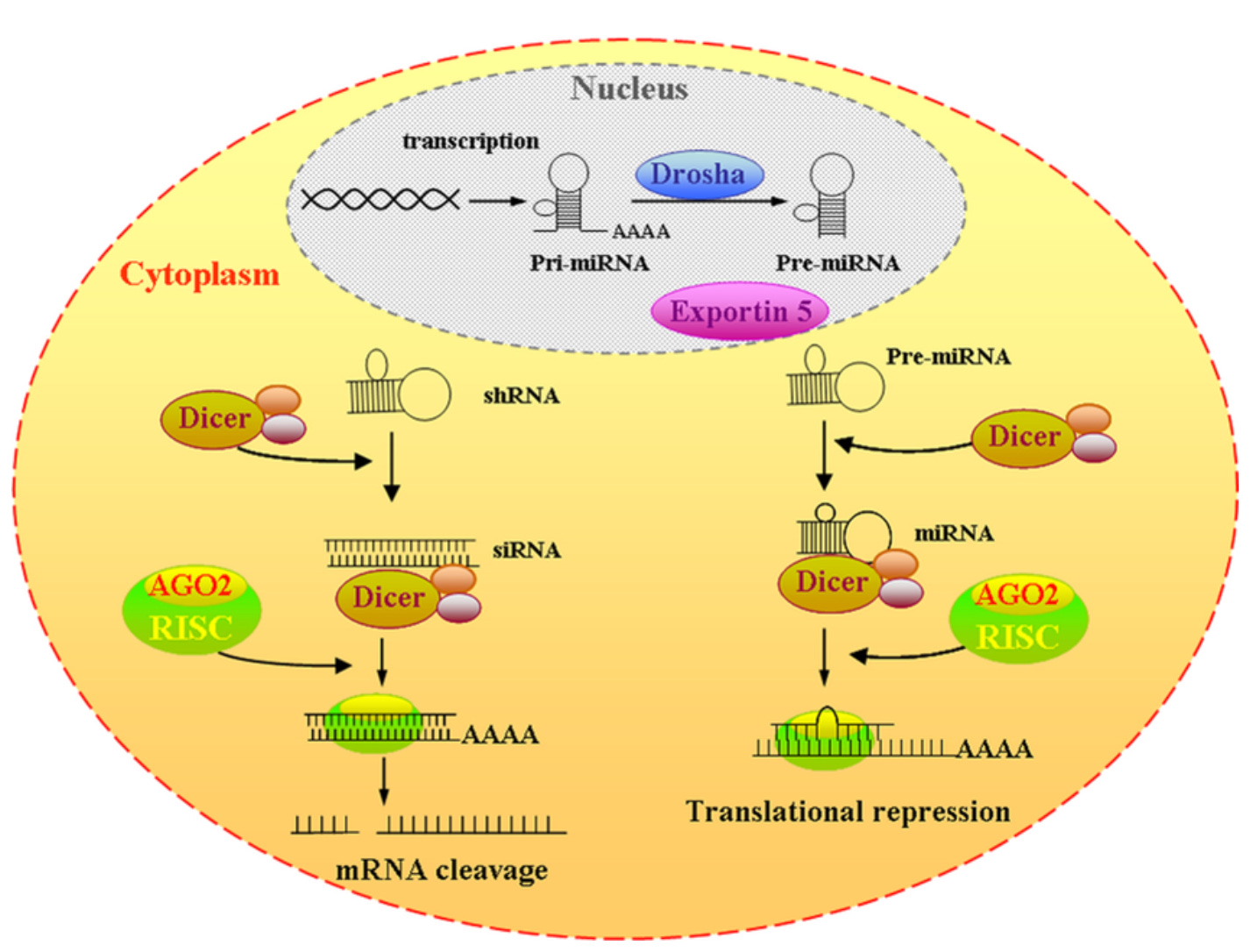
Two types of naturally occurring RNA have received attention for their potential or actualized therapeutic capabilities: siRNA and miRNA. Both exist primarily to prevent certain mRNAs from being translated into proteins, both are similar lengths (~20-24 nucleotides) and both make use of cells’ RNAi (or RNA interference) pathway. There are important differences: siRNA is double-stranded, has high specificity, and primarily leads to mRNA degradation. miRNA is single-stranded, has greater potential for imperfect binding (and thus for off-target effects), and primarily inhibits mRNA translation rather than encourages degradation. There’s also a non-naturally occurring approach to modulate mRNA expression, antisense oligonucleotides (or ASOs). ASOs are short, synthetic, single-stranded DNA or RNA strands that don’t take advantage of pre-existing RNAi machinery but do bind to mRNA and either inhibit translation or precipitate mRNA degradation. Tofersen, developed by Ionis and Biogen, is an FDA approved ASO treatment for a subset of ALS patients that initiates degradation of mutant SOD1 mRNAs. Vyondys 53, developed by Sarepta, is an FDA approved ASO treatment for a subset of DMD patients that binds to mRNA and prevents translation taking place.1
At a high level, the RNAi pathway that miRNA and siRNA are part of, and that therapeutics try to take advantage of, is straightforward enough. In the case of siRNA, the process typically kicks off with a double-stranded RNA (whether from a virus or otherwise) entering the cytoplasm. A dicer enzyme then cleaves that double-stranded RNA into a shorter ~20-24 length-ish fragment, which we term an siRNA. That siRNA then joins a group of proteins known as the RNA-induced silencing complex, or RISC. Next, one of the RNA strands (termed the passenger strand) is degraded, and the siRNA guide strand binds to mRNA and prevents translation. Unlike siRNAs, miRNAs don’t come from an endogenous source, and so are transcribed in a cell’s nucleus. miRNA is initially transcribed into a long, single-stranded, pri-miRNA, which is then cleaved by the Drosha enzyme into pre-miRNA (those are two different things rather than a typo!) This pre-miRNA then exits the nucleus and, like siRNA, is cleaved by the dicer enzyme into miRNA. Again like siRNA, this miRNA then joins the RISC complex, the passenger strand is degraded, and the miRNA goes onto prevent translation.
Thus far, only siRNA-based therapeutics and ASOs have received FDA approval. Alnylam has been a real powerhouse on the siRNA side. Its drug Onpattro, for the treatment of hATTR, was the first FDA-approved drug to leverage siRNA. hATTR is caused by a mutation in the gene that codes for the TTR protein, so Onpattro functions by binding to wild-type and mutant TTR mRNA to prevent subsequent protein expression. The company’s a true RNA platform, and since Onpattro’s approval has brought five more siRNA-based drugs to market. It’s worth noting that Alnylam’s products are delivered as siRNA, rather than as longer double-stranded RNA that first must be cleaved by the dicer. This is the standard approach for siRNAs used therapeutically.
miRNA-based therapeutics have not yet enjoyed the same level of success, which has been driven by a few factors. The first is its greater potential for off-target effects. This is driven by miRNA’s intrinsic tolerance for imperfect binding, as well as occasional loading of the passenger strand, rather than the guide strand, into the RISC. In both cases, this leads to suppression of the wrong transcript. The second reason is that, historically, exogenously delivered miRNAs have ended up boxing out endogenous miRNAs, which in turn really disrupts a cell’s regular functioning. In short, a cell’s RNAi machinery is busy enough working with the exogenous miRNA that it neglects to process its own miRNA. This results in abnormal levels of gene expression, which is a real problem!
UniQure has devoted a lot of effort towards solving these challenges with its miQURE platform. The company received a lot of press recently thanks to its pivotal Phase I/II study data for AMT-130 and the FDA’s flip flop on the drug’s accelerated approval pathway. AMT-130 is a treatment for Huntington’s, a severe neurodegenerative disease caused by too many CAG repeats in exon one of the HTT gene. This in turn leads to nerve cell damage in the brain.2 For the most part, those with Huntington’s will start to develop symptoms at between 30-50, and live ~15-20 years after initial signs of the disease. What begins as small involuntary movements gradually progresses to losing the ability to walk or talk, psychosis, and severe loss of cognitive function, among other things. Late-stage patients require around the clock care, and there is currently no cure to the disease nor a way to slow its progression. AMT-130 contains the genetic material for an miRNA that binds to the HTT transcript, thus preventing protein expression.
UniQure’s basic insight with its miQURE technology was to use an atypical miRNA scaffold, miR-451, that isn’t processed by the Drosha and Dicer enzymes. In other words, this miR-451 doesn’t follow the process that was laid out above, and thus should avoid the risk of overloading the cellular machinery. miR-451 also ‘is produced without the complementary passenger strand present, significantly reducing the rate of off-target effects.’3 Consequently, UniQure’s side-stepped two significant issues with miRNA-based therapeutics. Now, one still has the risk of off-target effects driven by miRNAs’ intrinsically imperfect binding to mRNAs. That requires less innovation to mitigate, and is dependent upon the specific miRNA sequence chosen to target a disease. In the case of AMT-130, UniQure tracked mRNA expression of transcripts similar enough to the mRNA transcript AMT-130 was meant to bind to, and found no marked changes in expression.4 The real innovation here is UniQure’s miQURE technology, rather than the company’s measuring of mRNA expression alterations for similar transcripts.
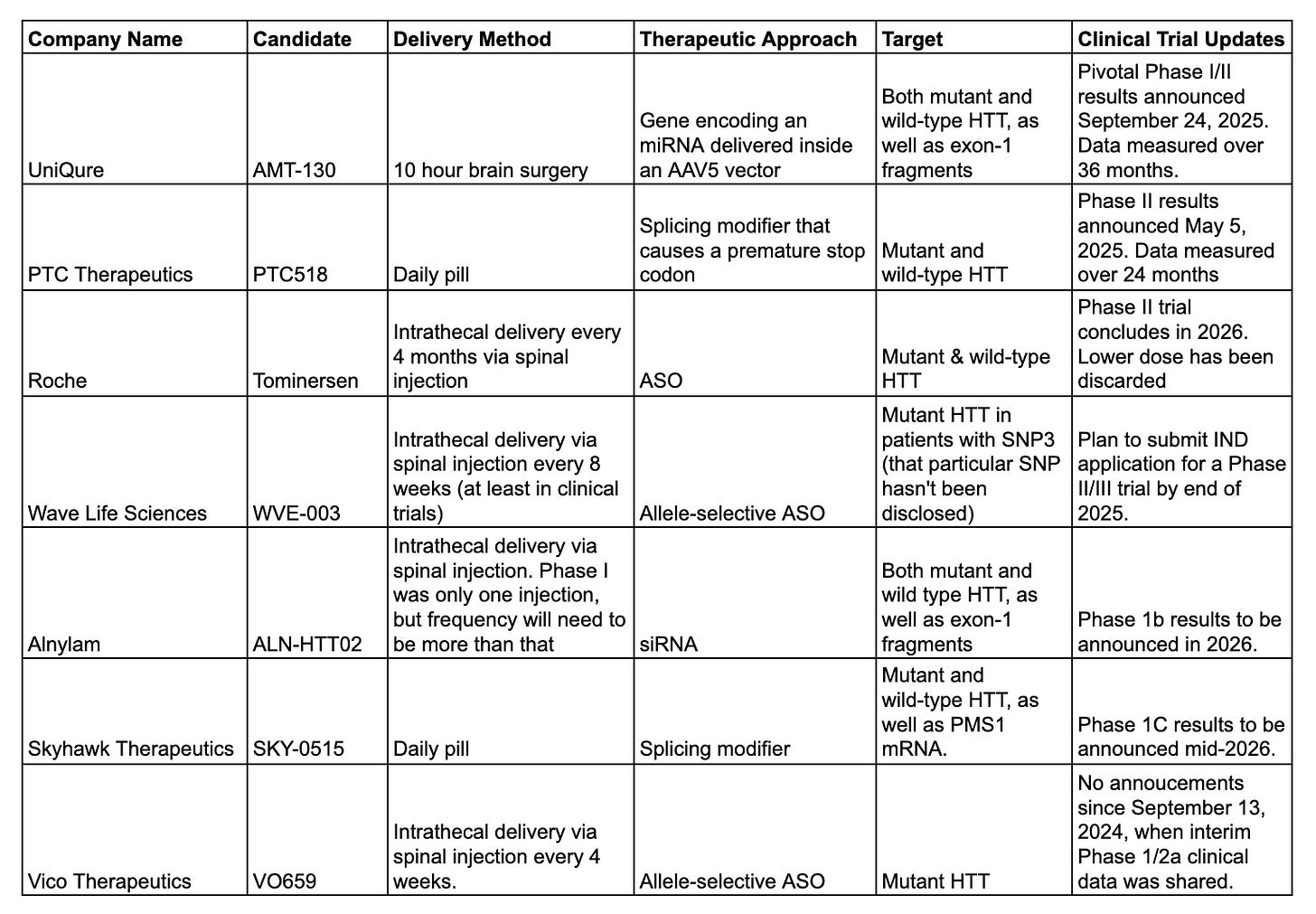
Now, UniQure’s technology being fascinating doesn’t mean that its AMT-130 candidate will actually work, nor that it will work better than competing approaches:
There are a few key takeaways here: UniQure’s candidate is further along in its clinical trials than competitors, its delivery method is the most complex, and PTC Therapeutics is one to watch in the short-term. UniQure being furthest along does really matter: this is a disease where there’s an enormous unmet need, and so being first to market is an advantage. It’s also a disease where progression is relatively slow, and so having data at 36 months after treatment rather than only after 24 is valuable for determining clinical effect. That said, its complex delivery method limits how quickly UniQure will be able to serve patients. There are ~68 centers in the U.S with the needed ClearPoint instrumentation, and the procedure has to be performed by a a neurosurgeon.5 That’s a contrast from intrathecal delivery, and even more of a contrast from PTC’s pill. However, investor excitement about PTC’s therapeutic has been more muted. The company did report a drop in blood HTT protein levels, but hasn’t shared the magnitude of the change in cUHDRS, other than saying there was one. cUHDRS measures actual Huntington Disease progression, and so while a drop in HTT levels could be encouraging it doesn’t mean a whole lot if there’s not a statistically significant change in cUHDRS.6 UniQure and Alnylam’s focus on targeting exon-1 fragments is worth mention: the CAG repeat expansion that causes Huntington also causes aberrant splicing that results in an exon 1 only transcript. This transcript is then translated into its own shortened protein, which accumulates in patients with the disease. There are researchers who believe you can’t have success slowing Huntington without inhibiting translation of these exon-1 fragments, so that’s something to keep in mind. I find Wave and Vico’s allele-specific approach to be fascinating: the wild-type HTT gene of course serves a purpose, so it’s reasonable to think silencing mutant and wild-type HTT translation could lead to harmful effects. Having said that, Wave Life Sciences had to nix two other allele-specific Huntington candidates targeting those with SNP 1 and SNP 2 mutations, so maybe there’s something about this approach that just doesn’t work.
Of course, how the FDA behaves is incredibly relevant to UniQure’s success, especially in the short-term. When UniQure released its Phase I/II results in late September the company planned on submitting a biologics license application (BLA) in the first quarter of ’26, with a potential US AMT-130 launch later on in the year. This schedule was based on previous discussions with the FDA on what would constitute primary evidence for an accelerated approval. Unfortunately, this timeline was completely thrown into question on Monday, when UniQure announced the FDA has now shifted the goalposts for an accelerated approval pathway. I don’t have anything to add here, other than it seems like an odd move for the FDA to make with a severe disease that doesn’t have any available treatments.
Disclaimer: The information in this post is not intended to be and does not constitute investment or financial advice. You should not make any decision based on the information presented without conducting independent due diligence.
Both of these drugs received accelerated approval from the FDA, and so do still need to confirm clinical benefit. Sarepta reported earlier this week that Vyondys actually failed to achieve a statistically significant change in the primary endpoint measured in the confirmatory trial, but that the company will still seek full FDA approval.
The effects occurring primarily in the brain are why so many treatment approaches are using intrathecal delivery and why UniQure is using brain surgery. It’s not easy to cross the blood-brain barrier!
UniQure AMT-130 presentation, pg 26. I haven’t taken a hard look at ClearPoint Neuro, but the 10 years out pitch is that if there’s explosion in gene therapies delivered via its instrumentation then the company will be a lot bigger than it is today.
HTT in the blood is also a lot easier to measure than HTT in cerebral spinal fluid. Because PTC’s therapeutic is delivered in pill form it’s expected to affect HTT expression levels throughout the body. Any Huntington therapeutic not delivered via pill, however, has to try and measure HTT levels in the CSF. Quanterix has an assay that does this, but there’s some question as to how accurate it really is. This was addressed in a recent interview with UniQure’s CEO & CMO: “There are also some pieces of the puzzle which are missing. This drug is designed to lower huntingtin levels, but there is no report in this update that the drug is working to do that – a feature of a drug known as target engagement. In part, this is perhaps because the current tools we have to measure huntingtin levels are quite noisy, which can make the results confusing”