Antibodies, Antibody Fragments, and Peptides: Targeting Muscular Diseases with RNA
Avidity, Dyne, PepGen, Entrada, and Arrowhead
Alnylam has been a great case study in the platform concept gone right. The company’s focused on developing RNAi therapeutics, initially for the liver, and has grown its menu of commercially available therapeutics from one in 2018 to six today. Alnylam’s also innovated on the delivery side of things. Its first FDA approved drug, ONPATTRO, used an LNP. Its more recent commercial therapeutics leverage GalNAc, enabling subcutaneous delivery and less frequent dosing.
An increasing amount of effort, from Alnylam and others, has focused on delivery methods that reach beyond the liver. The appeal of this is straightforward: there are plenty of extra-hepatic diseases that could be treated with nucleic acid approaches; it’s just a question of reaching the relevant tissue types. Capstan is an example of this. The company’s designed an antibody fragment conjugated LNP that accumulates in the spleen rather than in the liver, and binds specifically to CD8+ T-cells.
Beyond the spleen, delivery to muscle cells is another area companies have put plenty of resources toward. Part of the rationale here has to do with existing FDA-approved treatments for DMD. Sarepta has three different FDA approved exon-skipping therapeutics, and yet it’s unclear how beneficial these treatments really are for patients. These exon-skippers do not use an antibody, antibody-fragment, or cell-penetrating peptide (CPP) to enable enhanced muscular delivery, and so it seems reasonable to think that conjugating a PMO with something that improves muscular delivery should enjoy a straightforward path to approval. There’s always science risk, but the regulatory risk is at least somewhat diminished. As a result, most of the companies working on nucleic acid therapies for muscular diseases have some sort of DMD exon-skipper in the works. All of them also have a treatment for DM1, another form of muscular dystrophy that, similar to Huntington’s Disease, is caused by an expanded number of trinucleotide repeats. In the case of DM1, patients have too many CTG repeats in the DMPK gene. This in turn causes a larger than usual DMPK pre-mRNA, which then inhibits various splicing proteins from doing their job. This inhibition of splicing proteins is why the effects of DM1 are so broad: the splicing proteins can’t do their job, which results in splicing errors for a multitude of transcripts, and in turn impacts a multitude of proteins. Said differently, the problem with DM1 isn’t necessarily with the mutated DMPK gene itself, but instead with the cellular machinery that it inhibits.1
DM1’s impact on splicing activity means that, for a therapeutic to work, it actually needs to enter a cell’s nucleus. This is an added layer of complexity. In the case of typical RNAi therapies, such as Alnylam’s, the goal is to affect the mature RNA transcript, and so therapeutics only need to get beyond the cell membrane and enter the cytoplasm. In the case of treatments for DM1 (and exon-skipping approaches for DMD), the goal is to affect the pre-mRNA. Suppressing expression of DMPK mRNA doesn’t help anything: there’d still be the same splicing errors at the pre-mRNA stage.
The same delivery problem applies to exon-skipping treatments for DMD, although for different reasons. Here the issue isn’t that the mutated dystrophin gene is affecting the splicing of other proteins but that the patient isn’t producing a functional dystrophin protein. Exon-skippers trick the cellular machinery into skipping over a mutated exon as pre-mRNA is processed into mRNA, resulting in (hopefully) at least some functional protein. These DMD and DM1 treatment approaches illustrate the same point. When developing targeted RNA therapies for muscular disorders the problem is actually two-fold: figure out how to effectively reach the muscles and figure out how to enter the nucleus.
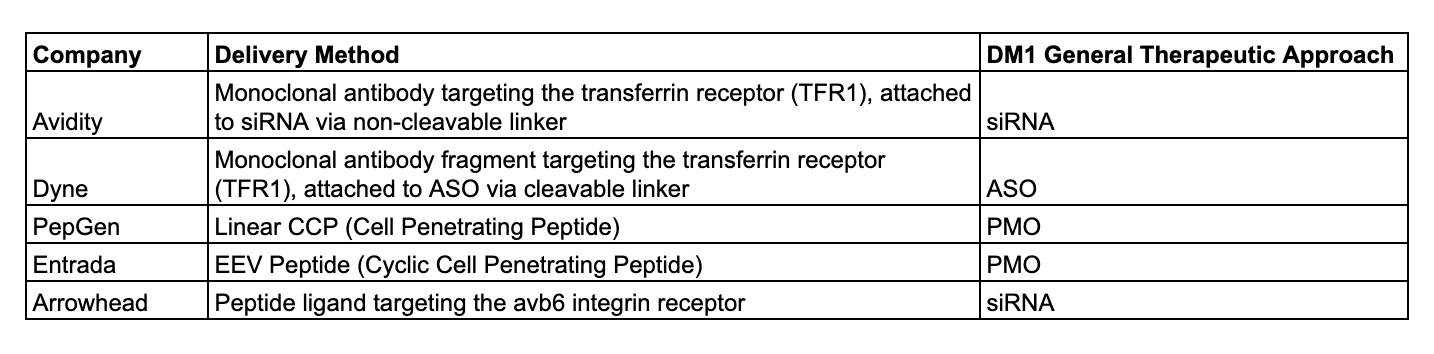
Thus far, there have been varied strategies for trying to reach the muscle cells:
Monoclonal antibodies are an obvious choice for two reasons: not only are there many existing FDA approved monoclonal antibodies, there are also plenty of FDA approved antibody-drug conjugates (although these are for treating cancer rather than genetic diseases). Consequently, the safety profile is pretty well understood.2 Historically, the issue with using mAbs to get to muscle cells has been around choosing which receptor to target. The downside of targeting TfR1 is that’s the receptor that transferrin primarily binds to. If transferrin can’t bind to TfR1, then your body doesn’t have a way to transport iron, and you’ll become anemic. Avidity engineered at antibody that shouldn’t interfere with this transferrin binding, but it’s not a total fix and they did still report some anemic patients.
Using an antibody fragment, as Dyne is doing, is also a somewhat obvious choice. While there are not yet FDA approved antibody-fragment conjugates of any kind, there are FDA approved standalone antibody fragment treatments, and plenty of antibody-fragment conjugates in clinical trials. Dyne’s decision is explained well in its annual report:
“We selected a Fab antibody over monoclonal antibodies, or mAbs, due to its potential significant advantages when targeting TfR1 to enable muscle delivery, including enhanced tissue penetration, increased tolerability due to lower protein load and reduced risk of immune system activation due to the lack of the Fc domain, the portion of an antibody that interacts with the immune system, on the Fab. To identify the proprietary Fab we use in our product candidates, we generated and screened proprietary antibodies for selectivity to TfR1 in order to enhance muscle specificity and for binding to TfR1 without interfering with the receptor’s function of transporting iron into cells. Binding to TfR1 may also enable delivery to the CNS.”3
All the above points are true. Any company that isn’t Avidity in this space is keen to point out the downsides of an antibody-based approach, particularly given the potential immune response. The magnitude of a patient’s immune response becomes very relevant in the case that Avidity’s treatment approach is correct in theory but hampered in practice by dose limitations because of the immune system.4 The point on tissue penetration is also interesting. All else equal, smaller proteins will have an easier time penetrating tissue than larger ones, and so it makes sense that an antibody fragment does better in this respect. The point I’d quibble with Dyne on is the benefits of not including an Fc domain in its fragment. While it lowers the risk of immune activation, it also negatively impacts a therapeutic’s half-life.
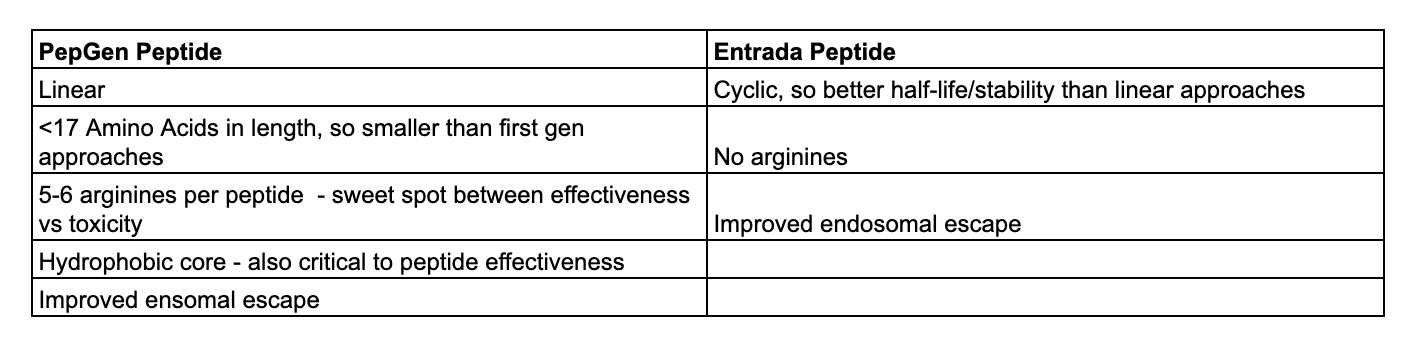
PepGen and Entrada are taking advantage of cell-penetrating peptides (CPPs), although in different ways. Using peptides as a delivery method has been appealing to researchers for quite some time, but first generation CPPs were found to be highly toxic. The more arginine residues a peptide had the more effectively it was able to penetrate cells, but also the more toxic it was in animal studies. As one would expect, PepGen and Entrada spend a good amount of time explaining how their peptides are different from the doomed first-generation instantiations.
Both companies emphasize their improved endosomal escape capabilities; first generation CPPs demonstrated very poor levels of endosomal escape, which is a bit of a problem. You can’t affect change in the nucleus if you can’t even get into the cytoplasm! More generally, it’s worth noting that peptides can cause kidney problems and hypomagnesemia. Until late last year Sarepta was actually developing a new version of its exon 51 skipping therapeutic that was conjugated to a peptide. The reported mean dystrophin increase was substantially better than its existing treatment (5.17%, so quite close to Dyne’s recent data, versus Sarepta’s existing <1%), but development was discontinued due to prolonged hypomagnesemia and declines in kidney function.
Arrowhead’s avenue to targeting the muscles is different from any of the above, and potentially has broader applicability. The company conjugates siRNA to a ligand that binds to the avb6 integrin receptor, which is mostly found on epithelial cells and has been used by Arrowhead in its pulmonary disease candidates. Historically, this receptor was thought to only be found on epithelial cells, but was then unexpectedly found present in skeletal muscle. Arrowhead also explored using antibodies to target muscles:
“So the reason we went with the integrin targeted approach and the advantages we see one, potential for improved knockdown, which we showed in the previous slide in 2 different species. And then additionally, we think that less drug is always better for the patients and the transferrin receptor targeted approach with an antibody oligo conjugate will require a higher total dose because siRNA is linked to this large monoclonal antibody compared with the integrin peptide targeted approach. For example, if you normalize for the siRNA dose, the amount of siRNA in a 12 mg/kg dose of ARO-DUX4 is equivalent approximately to the amount of siRNA in a 100 mg/kg of a DUX4 antibody oligo conjugate. And we see that this is an advantage, potential efficacy advantage, potential safety advantage and a potential advantage in terms of cost of goods.”5
In other words, much like PepGen and Entrada they emphasize the ability to take dosage higher. The quirk I’d mention with Arrowhead’s strategy is that using the avb6 integrin receptor means there’s ample opportunity for off-target effects – the therapeutic payload is not only ending up in the muscle cells.
When it comes to developing improved exon-skipping therapeutics for DMD, there’s not a real difference in approach between companies other than the delivery mechanism. There may be a difference in the exons being targeted, but the theory is all the same: prevent the RNA machinery from including a faulty exon in the mRNA transcript.
With DM1 treatment approaches, however, there are some interesting differences. As said above, DM1 is caused by too many CTG repeats in the DMPK gene. These repeats negatively affect a cell’s splicing ability, which in turn negatively impacts multiple proteins. In my view, Avidity, Dyne, and Arrowhead use a somewhat blunter strategy to combat DM1 by trying to reduce DMPK RNA expression overall. The less DMPK that’s expressed, the less harmful CTG repeats will be present in the nucleus, and the less a cell’s splicing machinery will be impaired. Entrada and PepGen, however, get more specific. Rather than reducing overall DMPK RNA expression, these companies focus on binding only to the expanded repeats. If PepGen/Entrada can get this to work it’s likely the better approach. The DMPK gene serves a purpose, so ideally you don’t want to be suppressing expression of its healthy, non-deleterious, portions. PepGen/Entrada’s approach isn’t totally dissimilar from what Wave Life Sciences is trying to do with Huntington’s. Rather than silencing both mutant and wild-type HTT, as companies like Alnylam and UniQure try to do, Wave instead tries to target only the mutated allele. In the case of Huntington’s, you still want the healthy HTT protein to be expressed!
It’s also worth mentioning the type of nucleic acid each company uses to affect gene expression. Specifically, it’s quite interesting that Arrowhead and Avidity both decided to use siRNA for their DM1 treatments. Typically, siRNAs are known for acting in the cytoplasm, and so you wouldn’t expect them to exhibit much activity in the nucleus. That said, both companies have reported some level of splicing correction, which indicates the siRNA is entering the nucleus somehow and at enough of a rate to display actual effectiveness. This is an interesting case of in practice being different from in theory, something that I’m sure is quite frustrating to see for anyone reading who’s a UChicago alum.
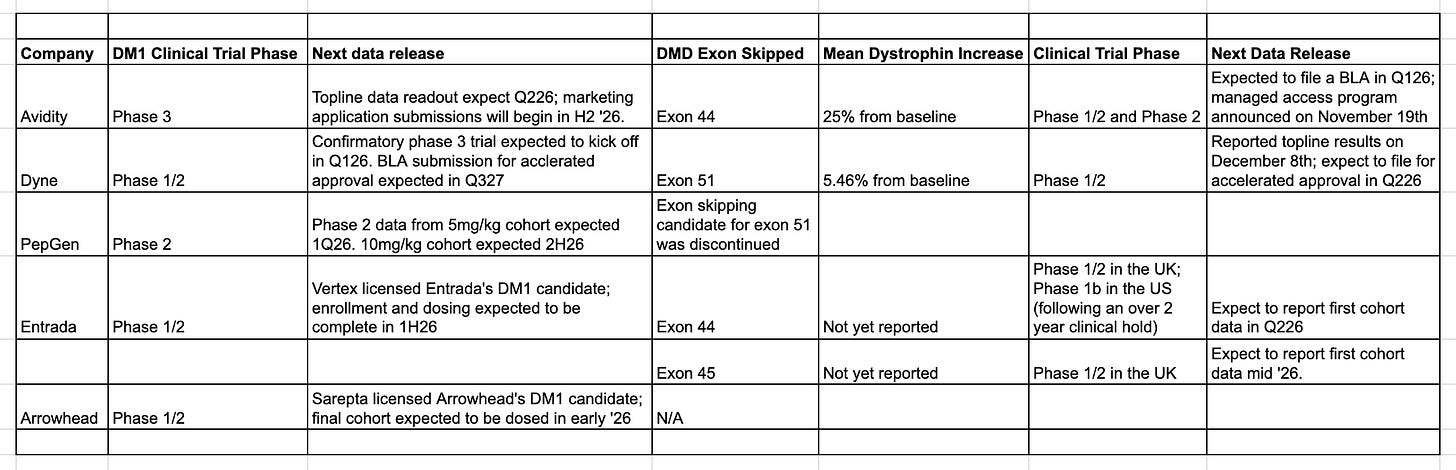
Below is a summary of where each company is in clinical trials for both DM1 and any DMD exon skippers:
There are a few points to mention. The first is that Avidity is furthest along in becoming a true platform. The company has an additional candidate in Phase 1/2 trials for treating FSHD (Facioscapulohumeral Muscular Dystrophy), and plans to submit a BLA for this candidate in 2H26. Dyne is close behind Avidity, but doesn’t yet have its FSHD candidate in clinical trials. At first glance Avidity’s exon-skipping data looks much better than Dyne’s, but that’s because exon 44 patients naturally produce more dystrophin. Both product candidates are exciting: if approved, Avidity’s exon 44 candidate will be the first to market for DMD patients with a confirmed exon 44 mutation. Ideally Dyne would be showing a dystrophin increase of greater than 10%, but 5.46% is significantly better than Sarepta’s EXONDYS 51. After halting progress on its exon 51 candidate given disappointing results, PepGen is now a single product company, but a very interesting one. For its DM1 candidate, they reported a mean splicing correction of 53.7% in phase 1 trials, a number that’s far above what either Avidity or Dyne have reported (16% and 27%, respectively). Critically for peptide-conjugated therapeutics, kidney issues were mild.6 Entrada’s work on cyclic peptides is fascinating, and management is eager to point out the theoretical advantages its approach could have against competitors. Its phase 1 exon 44 data didn’t surface any kidney issues, which is encouraging. That said, actual clinical data on efficacy is quite important here!
Disclaimer: The information in this post is not intended to be and does not constitute investment or financial advice. You should not make any decision based on the information presented without conducting independent due diligence.
This is why you see DM1 companies talk about freeing up MBNL1, a splicing protein whose behavior is inhibited by the expanded DMPK gene. If you can restore MBNL1’s function you should be able to fix a lot of the splicing errors.
If you’re Entrada, PepGen, or Arrowhead, you’ll argue that the safety actually isn’t that well understood.
Dyne 2024 Annual Report, pg 4.
Entrada will argue this is the case for Avidity’s exon 44 therapeutic, and that Entrada will be able to drive a higher dystrophin increase because they are (theoretically) not as worried about an immune response. This is currently very much in theory, because Entrada has the potential to cause kidney toxicity with too high a dose. That said, perhaps clinical trials will show that not to the case!
Transcript from Arrowhead’s May 2024 Summer Series R&D Webinar.
There were some safety issues reported for PepGen’s now discontinued DMD candidate, but management put that down to the combined effects of PepGen’s candidate plus drugs DMD patients are already on.


Really sharp breakdown of the delivery tradeoffs here. The point about antibody-conjugated therapies having higher protein loads (like 100mg/kg vs 12mg/kg for peptide-ligand approaches) is huge from a safety and COGS perspectiv. I've been tracking Arrowhead's integrin strategy and the off-target concern is valid but the efficiency gain is tempting. One thing that suprised me was PepGen's 53% splicing correction vs Avidity/Dyne's 16-27 percent, tho kidney tox is obviously the major question mark there.